Late at night, a young professional sits on her couch, tissue box beside her, eyes watering as she types “best cure for nasal allergy” into YouTube. Within seconds, hundreds of cheerful faces appear on the screen, some recommending herbal teas, others promising quick fixes or miracle nasal sprays. She clicks the one with the most views. The advice sounds convincing, but is it correct? Millions of people worldwide do the same every day, trusting online videos more than medical consultations. A new study led by Dr. Sanjay Kumar, published in the Journal of Otolaryngology and Head & Neck Surgery, takes a closer look at what they actually find, and what that means for public health.
The rise of the “YouTube doctor”
Allergic rhinitis, commonly known as hay fever or nasal allergy, affects millions of people, often year-round. It causes sneezing, itching, nasal congestion, and fatigue, disrupting sleep and work. Although the condition is easily managed with antihistamines, nasal corticosteroids, and, in some cases, immunotherapy, patients increasingly turn to the internet for instant solutions. Among social media platforms, YouTube has emerged as the most popular source of health information, reaching billions with its mix of personal stories and persuasive visuals.
This easy accessibility has blurred the boundary between expert advice and personal opinion. To understand how this shift affects patients, Dr. Kumar and his colleagues conducted a detailed content analysis of the most-viewed YouTube videos on the management of allergic rhinitis. Their goal was to assess the reliability, balance, and practicality of this online information.
Turning clicks into data
The research team systematically searched YouTube using neutral keywords such as “allergic rhinitis treatment,” “nasal allergy remedy,” and “hay fever management.” They selected fifty English-language videos that focused specifically on treatment and met quality criteria for audio, visuals, and relevance. Each video was carefully evaluated using three validated instruments: DISCERN for reliability and balance, JAMA benchmarks for transparency, and the Patient Education Materials Assessment Tool (PEMAT) for understandability and actionability.
The team also documented the number of views, likes, and comments, as well as the creator of each video: medical professionals, influencers, pharmaceutical companies, or alternative healers. By comparing engagement metrics with quality scores, the researchers aimed to answer a crucial question: Does popularity reflect reliability, or are viewers rewarding style over substance?
Who owns the conversation?
The analysis revealed that influencers dominate the space. Nearly half the videos were created by non-medical personalities who share lifestyle tips or personal experiences. While these videos attracted the highest viewership, they often scored lowest for factual accuracy. Videos created by medical professionals, although fewer in number, demonstrated strong adherence to evidence-based guidelines and achieved the highest reliability scores. Pharmaceutical and corporate channels occupied the middle ground, while alternative-therapy videos had the weakest educational value.
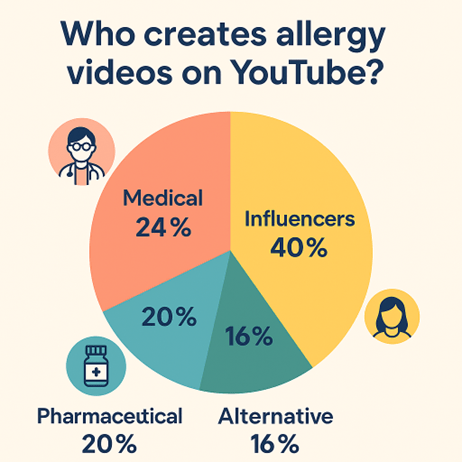
The findings make it clear that the loudest voices on social media are not necessarily the most trustworthy, and that medical expertise is often drowned out by confidence and charisma.
Online videos can empower patients but only when science leads the story.
– Sanjay Kumar
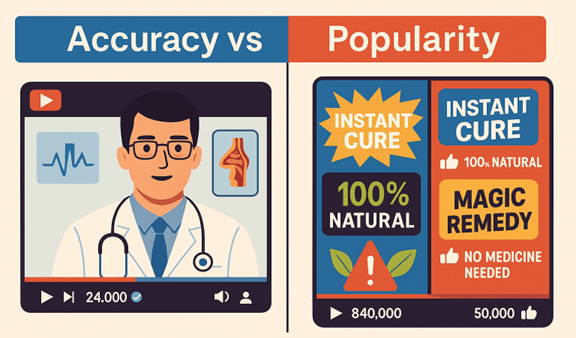
When popularity beats accuracy
Perhaps the most striking discovery was the inverse relationship between quality and popularity. Videos with the highest DISCERN and JAMA scores tended to have modest view counts, while those with weaker evidence attracted millions of views. Roughly one in three videos contained misinformation ranging from exaggerated claims about herbal cures to unfounded fears about nasal steroids or immunotherapy. Such videos may appear harmless, but they subtly shape patient expectations and self-treatment choices.
Many creators emphasised short-term comfort measures, such as steam inhalation, saline rinses, or dietary changes, while neglecting long-term strategies, including immunotherapy. While these remedies can complement medical care, presenting them as complete solutions can delay diagnosis and proper management. The study underscores a persistent truth: algorithms favour engagement, not accuracy.
What patients actually hear
When the team examined how the videos communicated, they found a clear divide. Educational and professionally produced content scored high on understandability and actionability, offering viewers practical steps and clear explanations. In contrast, testimonial videos where individuals shared personal “success stories” scored the lowest. These often relied on anecdote and emotional appeal, with little or no reference to medical evidence.
Audience engagement mirrored this difference. The most liked videos were those that simplified complex ideas or offered quick comfort, rather than promoting scientifically sound advice. This pattern reveals a communication gap: patients value clarity, while experts prioritise accuracy. The best health education needs both.
Why it matters beyond allergies
Allergic rhinitis might appear trivial compared with other chronic illnesses, but its global burden is substantial. If misinformation spreads even in such a common and well-understood condition, the implications for more serious diseases are troubling. YouTube’s influence extends far beyond allergy management; it shapes how people perceive medical authority and risk.
The study’s findings highlight a larger issue: health information online is governed by algorithms optimised for attention, not truth. This poses a challenge for healthcare professionals, who must compete not just in clinics but in the digital marketplace of ideas.
Bridging the credibility gap
The research points toward an opportunity rather than despair. Clinicians and hospitals can use the same medium of short, visually engaging videos to reach patients directly. Three-minute explainers on how to use nasal sprays correctly or when to seek immunotherapy could gain traction if crafted with empathy and clarity.
He advocates for collaboration between doctors, digital creators, and public health communicators to ensure that quality information is both credible and compelling. Platforms like YouTube can also play a proactive role. By verifying medical professionals and curating playlists based on established guidelines, they can help steer viewers toward trustworthy content without limiting access.
Accuracy doesn’t have to be dull. The challenge is to make science simple without making it shallow.
– Sanjay Kumar
A public-health opportunity
The findings align with global efforts to promote digital health literacy. Governments and professional societies can develop voluntary transparency codes for online health communication, requiring authorship disclosure, date of publication, and references to credible sources. Such steps could elevate the baseline quality of online content and help users make informed choices.
Medical education must also evolve. Training young clinicians to communicate effectively on social media will be as important as teaching them surgical or diagnostic skills. Hospitals could treat online education as part of patient care, recognising that a well-informed public reduces clinical burden and improves outcomes.
Learning to trust again
For millions who suffer from sneezing fits and sleepless nights, allergic rhinitis is more than a seasonal nuisance; it’s a reminder of how fragile trust in medical information has become. When anyone with a camera can claim to be an expert, distinguishing evidence from opinion becomes challenging. The path forward lies in partnership: between patients who seek clarity and doctors who offer it, between technology platforms and medical science, and between curiosity and caution.
As Dr. Kumar concludes, “Our responsibility doesn’t end in the clinic. It extends to every screen where someone is looking for relief.” The question that remains is whether we can make the digital space as safe, evidence-based, and humane as the best hospital consultation room.
Reference
Kumar, S., Dutta, A., Vallur, S., & Singh, R. (2025). A Content Analysis of YouTube Videos on Allergic Rhinitis Management. Indian Journal of Otolaryngology and Head & Neck Surgery. https://doi.org/10.1007/s12070-025-05396-6