Depression remains one of the most disabling health conditions worldwide, yet access to high-quality psychological therapy continues to lag behind demand. In this context, digital mental health tools have been promoted as a scalable solution. A new large randomised controlled trial published in the Journal of Medical Internet Research has examined whether artificial intelligence-powered natural language feedback can improve engagement and outcomes in fully self-guided internet-based cognitive behavioural therapy. The study, led by Mirai So from Tokyo Dental College, provides one of the most rigorous tests to date of how AI-driven empathy performs in real-world mental health interventions.
Titled “Effect of AI-Based Natural Language Feedback on Engagement and Clinical Outcomes in Fully Self-Guided Internet-Based Cognitive Behavioral Therapy for Depression”, the research involved more than 1,100 adults and offers nuanced evidence. While AI did not dramatically outperform standard online therapy in symptom reduction, it substantially improved user participation. For digital health innovators, clinicians and policymakers, these findings raise important questions about how emotional interaction with machines may shape the future of mental health care.
Why digital mental health still struggles with engagement
Internet-based cognitive behavioural therapy, often abbreviated as iCBT, has become a cornerstone of digital mental health strategies. It offers structured therapeutic content, cognitive restructuring exercises, and psychoeducation without requiring face-to-face sessions. Previous meta-analyses have shown that iCBT can reduce depressive symptoms, but the benefits are often smaller than those seen in therapist-guided programmes. A central reason is poor adherence. Many users abandon programmes before completing even half of the recommended sessions.
Self-guided mental health interventions rely heavily on sustained motivation, self-discipline, and emotional resilience. Without human feedback, users frequently disengage when exercises become cognitively demanding or emotionally uncomfortable. In a real-world usage analysis of 93 mental health apps, the median 15-day retention rate was reported to be only 3.9%, highlighting the substantial challenge of sustaining user engagement in self-guided interventions.
As a result, researchers have begun exploring whether artificial intelligence, particularly natural language processing, can replicate some elements of human therapeutic support. The trial conducted by Mirai So and colleagues was designed specifically to isolate the contribution of AI feedback in this context.
Inside the study design and participant population
The research team recruited 1,187 adults aged between 20 and 60 years through an online panel in Japan. Participants were randomly assigned to one of three groups. One group received AI augmented iCBT, another received the same iCBT programme without AI feedback, and the third group was placed on a waitlist control. Importantly, the two active intervention groups were identical in content. The only difference was the presence or absence of AI-driven natural language feedback.
The AI system, developed in collaboration with NEC Solution Innovators, analysed user input during cognitive restructuring exercises and generated two types of responses. The first was empathic feedback, designed to acknowledge emotional content and validate user experiences. The second was advisory feedback, offering guidance on completing tasks correctly. The entire programme was delivered online and consisted of six weekly sessions combining video-based psychoeducation with structured exercises. In the non-AI condition, participants received neutral, content-agnostic acknowledgment only, and the study employed a double-blind design in which participants were unaware of their group assignment.
Baseline depressive symptoms were assessed using the Patient Health Questionnaire-9, a widely used clinical screening tool. Follow-up assessments were conducted immediately after the intervention and again three months later. This design allowed the researchers to evaluate both short-term and sustained effects of AI-supported digital therapy.
Engagement emerges as the strongest benefit
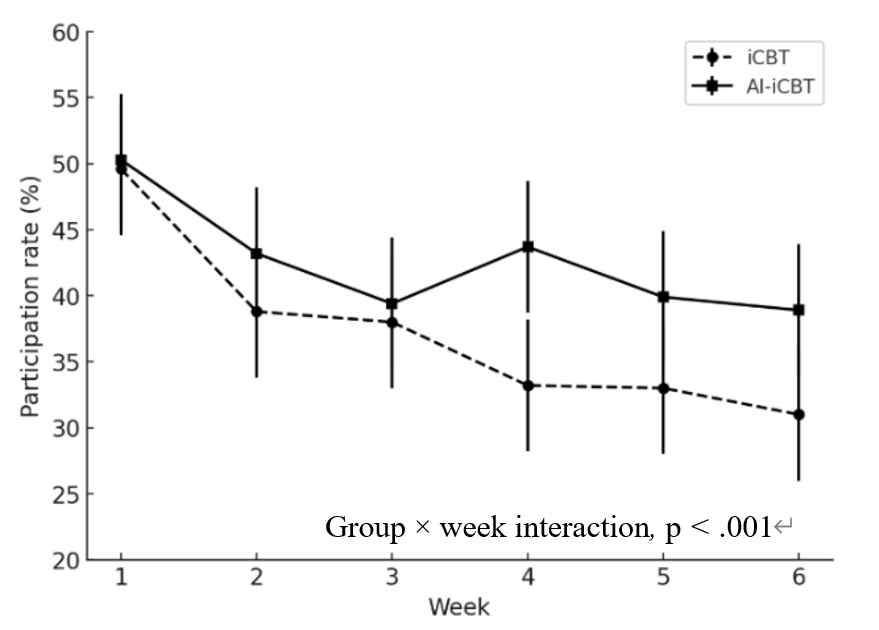
One of the clearest findings from the trial was the impact of AI on engagement. Weekly participation rates declined steadily in both intervention groups, a pattern commonly observed in digital health studies. However, participants receiving AI-augmented iCBT were significantly more likely to continue completing exercises over time. Statistical analysis showed a 23 percent higher odds of weekly participation compared with the non-AI group .
By the sixth week of the programme, around 40 percent of users in the AI group were still actively engaging with the platform, compared with roughly 30 percent in the standard iCBT group. While these figures still reflect substantial dropout, the relative improvement is notable. For population-scale interventions, even modest increases in adherence can yield substantial public health benefits.
The empathy effect and human-like interaction
Perhaps the most striking result emerged from the exploratory analysis of AI functions. When the researchers examined which type of feedback most strongly predicted continued participation, empathic responses stood out. Participants who received empathic AI messages during their first session had nearly tenfold higher odds of remaining engaged in subsequent weeks (odds ratio = 9.9).
In contrast, advisory feedback that focused on task correction and instructional guidance showed no statistically significant association with engagement. This suggests that emotional validation, rather than technical support, plays a dominant role in sustaining motivation. Even when delivered by an algorithm, empathic language appears to foster a sense of being understood, which may reduce feelings of isolation commonly experienced by people with depression.
This finding aligns with broader research on digital mental health chatbots and conversational agents. Previous studies have shown that perceived empathy and relational warmth improve therapeutic alliance, even in automated systems. The current trial adds robust experimental evidence to this emerging field by demonstrating that empathic AI feedback is not only appreciated by users but also actively changes participation behaviour.
Testing the effects of empathy through AI in a functionally double-blind way is a major step forward. The findings extend beyond digital health to fields such as education and marketing, offering new perspectives on how we work with AI—and how we rethink face-to-face psychotherapy as well.
– Mirai So
What this means for the future of digital CBT
Digital mental health services are expanding rapidly, driven by workforce shortages, rising demand and the growing acceptance of telehealth. Fully self-guided interventions remain the most scalable option, but their effectiveness is limited by low completion rates. The integration of AI-driven natural language processing may help address this structural weakness.
Rather than focusing solely on symptom prediction or diagnostic automation, this research emphasises the behavioural dimension of artificial intelligence in healthcare. The ability of AI systems to sustain engagement, promote adherence and create emotionally supportive interactions could be just as valuable as direct clinical effects. In practical terms, this may influence how future digital therapeutics are designed, shifting attention towards user experience, conversational design, and emotional responsiveness.
For clinicians and researchers, the findings also raise important ethical and regulatory considerations. If AI-mediated empathy becomes a standard component of mental health platforms, questions about transparency, user trust, and algorithmic accountability will require careful management.
Limitations and real-world challenges
Despite its scale and methodological rigour, the study has several limitations. Most participants were recruited from an online research panel and had relatively high digital literacy. Only a small proportion were actively receiving mental health treatment, which may limit generalisability to clinical populations. In addition, overall dropout rates remained high across both intervention groups, underscoring the persistent difficulty of maintaining long term engagement in self guided programmes .
There were also technical limitations, including missing session-level symptom data due to software issues. Furthermore, the study population was restricted to Japanese-speaking users aged under 60, which may limit its applicability to other cultural contexts and to older adults. The authors emphasise the need for replication studies in diverse settings before drawing definitive conclusions.
Reference
So, M., Sekizawa, Y., Hashimoto, S., Kashimura, M., Yamakage, H., & Watanabe, N. (2026). Effect of AI-based natural language feedback on engagement and clinical outcomes in fully self-guided internet-based cognitive behavioral therapy for depression: A 3-arm randomized controlled trial. Journal of Medical Internet Research, 28, e76902. https://doi/10.2196/76902