When a scientific study tracks the long-term safety of stem cell infusion in healthy adults, it marks a rare moment in regenerative medicine. This is why a newly published paper titled Umbilical Cord-derived Mesenchymal Stem Cells (CLV-100) Infusion in Healthy Subjects: a 5-Year Follow-Up Study on Safety and Immunomodulatory Effect by Sze Piaw Chin and his coauthors has sparked renewed attention. The work, published in Regenerative Engineering and Translational Medicine (link), reports outcomes from a five-year clinical follow-up of volunteers who received a single infusion of umbilical cord-derived mesenchymal stem cells, or UCMSCs.
Led by Prof. Dr. Sze Piaw Chin of Cytopeutics Sdn Bhd, the research was conducted in collaboration with the M. Kandiah Faculty of Medicine and Health Sciences at Universiti Tunku Abdul Rahman and CMH Specialist Hospital. Although stem cell research has expanded rapidly over the past two decades, long-term human safety data remain scarce, particularly in individuals without underlying disease. For this reason, the findings offer important insights into how UCMSCs behave in the human body over extended periods.
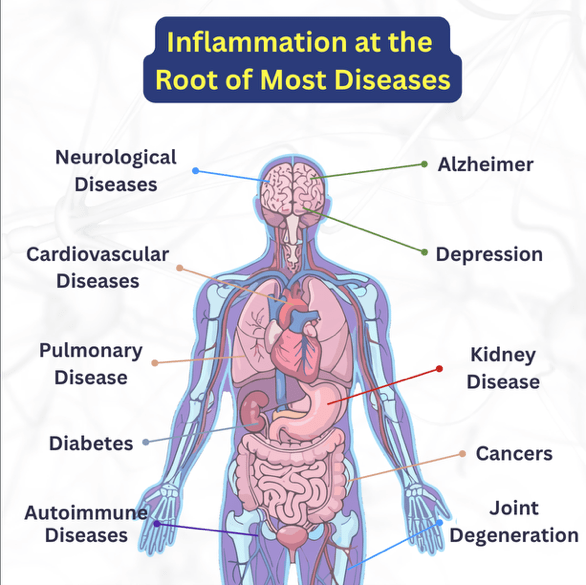
Stem cell therapy is frequently discussed as a frontier for treating chronic inflammation, autoimmune disease, and age-related frailty. However, safety concerns and inconsistent clinical evidence have slowed progress. This study, therefore, provides a detailed contribution to a field often clouded by speculation and commercial misuse. It does not promise miracle cures, but it builds an evidence base for therapies that modulate the immune system in controlled and predictable ways.
Why umbilical cord stem cells matter
Umbilical cord-derived mesenchymal stem cells have become a preferred cell source in regenerative medicine due to their abundance, ease of isolation, and low immunogenicity. They release a secretome that contains proteins, cytokines, and growth factors capable of modulating inflammatory pathways. Their application spans cardiovascular disease, diabetes, autoimmune disorders and chronic wound management.

The current study focuses on a specific UCMSC product known as CLV-100, developed by Cytopeutics. Earlier work demonstrated that a single intravenous infusion of CLV-100 was safe up to six months and produced a dose-dependent immunomodulatory effect. The present study builds on that evidence by assessing what happens to the immune system, organ health and inflammatory markers five years after infusion.
This is valuable because long-term immune modulation can have both beneficial and harmful effects. Persistent suppression might increase susceptibility to infection, while chronic stimulation may accelerate inflammatory diseases. Understanding where UCMSCs fit on this spectrum is essential before they can be adopted more widely.
Inside the five-year follow-up
The research team tracked 11 healthy volunteers who had received either a low dose of 65 million cells or a high dose of 130 million cells. These doses correspond roughly to one or two million cells per kilogram of body weight. All participants returned for follow-up visits where clinicians performed clinical examinations, lung function assessments, and extensive blood testing, including full blood counts, metabolic markers, tumour markers, and inflammatory cytokines.
A particular emphasis was placed on immune-related biomarkers, including IL-6 and TNF-alpha, which promote inflammation, and IL-1 receptor antagonist, which reduces inflammatory signalling. The team also monitored growth factors, including hepatocyte growth factor, vascular endothelial growth factor, and transforming growth factor beta, which influence tissue repair, angiogenesis, and immune balance.
The volunteers ranged in age from 46 to 82 years at the start of the study. Importantly, none dropped out, making it one of the few stem cell studies with complete long-term retention. This increases confidence in the stability of the findings.
What remained stable and what changed
One of the strongest observations was sustained safety. Across the entire cohort, no major health complications, hospitalisations or treatment related adverse effects were recorded. Clinical markers for liver, kidney and metabolic health remained within normal ranges, including in participants over 60 years of age. Tumour markers also stayed normal, with no indications of malignancy.
These results address a common concern in regenerative medicine. There is persistent anxiety around tumourigenicity due to the proliferative capacity of stem cells. According to the biomarker trends in this study, there was no evidence that CLV-100 triggered tumor formation, even five years later.
Some parameters shifted slightly, but these changes aligned with natural aging patterns. Lung function declined modestly, which is expected in older adults. Insulin levels rose slightly, although they remained within normal limits. Erythrocyte sedimentation rate increased but did not indicate pathological inflammation. Such observations reinforce that the physiological trajectories of these individuals were typical rather than treatment-driven.
A persistent imprint on the immune system
Where the findings become particularly intriguing is in the patterns of inflammatory cytokines. The high-dose group showed a striking and durable reduction in the pro-inflammatory cytokines IL-6 and TNF-α. Levels fell from moderately elevated values at baseline to within normal ranges after five years. At the same time, IL-1 receptor antagonist increased significantly, suggesting a long-lasting tilt toward an anti-inflammatory state.
For researchers studying chronic inflammation or metabolic disorders, these observations are notable. Persistent low-grade inflammation is associated with cardiovascular disease, arthritis, diabetes, and neurodegeneration. The ability of a single stem cell infusion to shift inflammatory profiles over such an extended period suggests a meaningful biological effect.
However, this effect varied by dose. The low-dose group did not show statistically significant changes in these biomarkers. This highlights the need to consider cell dose as a critical factor in UCMSC therapy design, a topic frequently discussed in the regenerative medicine community.
Growth factors also changed in a pattern that suggests improved immune balance. Hepatocyte growth factor and vascular endothelial growth factor declined to within normal ranges, reducing the risk of unwanted angiogenesis or inflammatory vascular changes. Transforming growth factor beta increased but remained within reported normal limits, reflecting healthy tissue remodelling processes.
These biological shifts align with the hypothesis that UCMSCs act primarily through paracrine signalling, releasing molecules that reprogramme immune cell behaviour rather than engrafting long-term.
-Sze Piaw Chin
Ageing, frailty and the search for healthier years
Aging research is increasingly focused on inflammation as a central driver of frailty and age-related disease. Higher levels of IL-6 and TNF-alpha are common in older adults and correlate with sarcopenia, cognitive decline, and metabolic dysfunction. The study, therefore, explored whether the long-term immune effects of CLV-100 differed between younger and older participants.
Interestingly, no major differences were reported. Older participants did not exhibit higher inflammation than younger volunteers at the five-year mark. Their organ function profiles were also similar. Although the sample size is small, the findings suggest a potential for UCMSC therapy to moderate inflammation associated with biological aging.
The authors caution that without a control group, the results cannot be definitively attributed to CLV-100. Lifestyle factors, physical activity, diet and social environment all influence ageing trajectories. Even so, the absence of age-related deterioration in inflammatory markers is a promising observation.
Caution and the road ahead
Although the results are encouraging, the study is not without limitations. The sample size is small and lacks a placebo controlled arm, which makes causal interpretation difficult. Follow-up data from years one to four are missing due to the COVID-19 pandemic. In addition, measuring cytokines with multiplex assays introduces variability compared with single target methods.
The authors remain careful in their conclusions. They do not claim therapeutic benefit for disease treatment, nor do they suggest immediate clinical application for frailty. Instead, they frame the results as evidence of safety and of a consistent immunomodulatory signature that warrants further study. This measured approach is important given the global concern about unregulated stem cell clinics and exaggerated claims around anti ageing therapies.
Future studies would need to include larger populations, diverse age groups, disease specific cohorts and more rigorous controlled designs. Combining biomarker analysis with functional metrics such as muscle strength, mobility or cognitive performance would also strengthen understanding of how UCMSC therapy influences the ageing process.
Reference
Chin, S. P., Ng, W. C., Tai, L., Mohd, M. A., Then, K. Y., & Cheong, S. K. (2025). Umbilical Cord-derived Mesenchymal Stem Cells (CLV-100) Infusion in Healthy Subjects: a 5-Year Follow-up Study on Safety and Immunomodulatory Effect. Regenerative Engineering and Translational Medicine. https://doi.org/10.1007/s40883-025-00384-2